Understanding the important work of the Nevada State Public Health Laboratory
Most of you probably know little about the work of the Nevada State Public Health Laboratory (NSPHL). You should know more, because the lab scientists and technicians are literally working around the clock to protect you and all Nevadans from a wide range of potential infections, food-borne illness, and unsafe water, as well as providing emergency response to biological and chemical terrorism, and testing every Nevada baby for more than 30 hereditary diseases.
Established in 1909, the NSPHL serves as Nevada’s centralized lab, representing a first line of defense in the rapid detection of a public health threat. The laboratory is part of the University of Nevada, Reno School of Medicine and located on the University campus.
Here are a few facts to help you understand the important work of the NSPHL and how it serves the entire state, so well. The laboratory performs over 550,000 tests each year to help keep Nevadans safe and healthy—that’s more than 2,000 tests each day. Over 400,000 of those tests are conducted on newborn babies, with each baby being tested twice in the first 10-14 days of life for conditions ranging from cystic fibrosis to congenital hypothyroidism to sickle cell disease to severe combined immunodeficiency disease. Every day, the NSPHL is confronted with questions and challenges, ranging from the safety of water in the Truckee River to outbreaks of whooping cough in local schools to whether the West Nile virus has come to Nevada.
The NSPHL is staffed by over 30 scientists and technicians, with a budget of over $7m/year. But, the cost per Nevada resident has dropped over the years, with state funding per capita declining from $644 in 1998 to $564 in 2018 due to an increasing level of efficiency and success by the laboratory management in seeking grants and contracts from other sources.
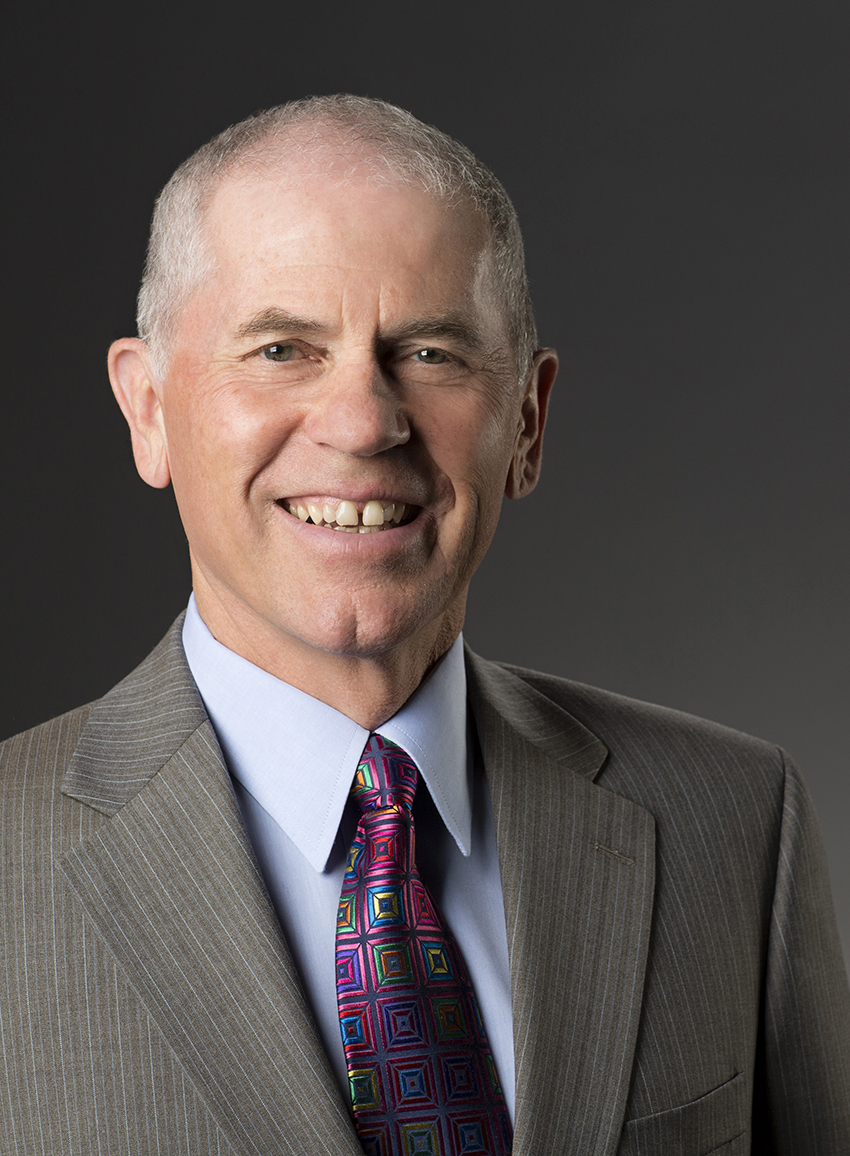
The NSPHL also has a new Director, Mark Pandori, Ph.D. Dr. Pandori has over 15 years of high-level experience in public health laboratory leadership, most recently as Director of the Alameda County Public Health Laboratory in Oakland, California. He earned his Ph.D. from the University of California, San Diego, completed a fellowship at Harvard University, and holds several certifications in diagnostics and public health microbiology. He will serve as a faculty member in the Department of Pathology and Laboratory Medicine at UNR Med where he will teach medical students and residents, in addition to his laboratory leadership responsibilities.
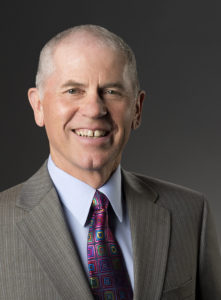
Dr. Pandori will continue the outstanding tradition of public health leadership that the state has enjoyed with Dr. Trudy Larson, professor and dean of the School of Community Health Sciences, who has served as NSPHL director since July 2014.
The NSPHL is an example of community service and engagement that characterizes the core mission of UNR Med at its best, to serve the state, to improve the health and quality of life and to contribute to a Healthy Nevada. Nevada residents can be confident that their public health is in good hands with the leaders and scientists at the Nevada State Public Health Laboratory.