By the time this article is published there will have been many updates and changes to the circumstances surrounding COVID-19 and the medical school experience, but today I’ll offer you a perspective from a moment in time as a 3rd year medical student navigating the spread of the novel coronavirus.
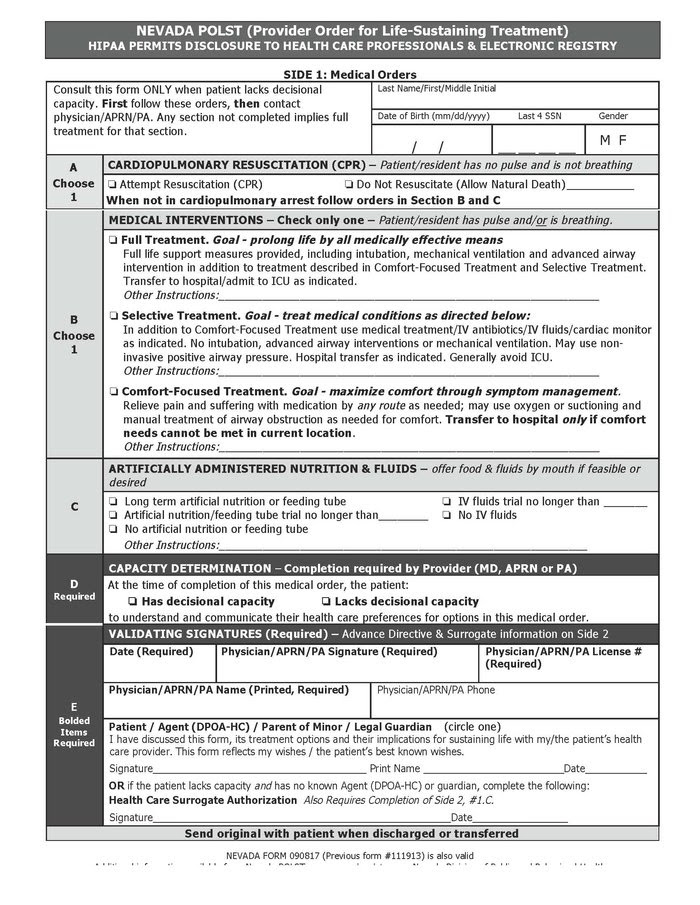
By mid-March all inpatient rotations were canceled for medical students. All clinical rotations for 3rd and 4th year students--inpatient and outpatient---were canceled until at least March 31 in a nationwide decision by the AAMC and LCME.
The impacts of the spread of this virus on medical education began slowly percolating. I remember first learning about the virus during my inpatient pediatric rotation when it was primarily in China. The floor was full of RSV patients and the whole team would put on their masks, gowns, and gloves and speak to the patients as we rounded. My colleagues on that same rotation now more than a month later have a very different experience. Medical students are barred from seeing patients on droplet precautions in order to preserve the hospital’s supply of PPE.
Hospitals in the region have completely restricted student access. And a source of anxiety for myself and my classmates is if we will be able to complete our clinical rotations and maintain our current timeline for graduation. At the same time that we are applying to 4th year away rotations in our desired specialties, we are getting notified of away rotation cancellations across the country.
There are different impacts felt at every level of medical school.
Our MS1s are trying to complete their anatomy requirements in an online capacity as UNR has made the decision all classes--graduate and undergraduate--will be online for the foreseeable future.
Our MS2s are in their dedicated study period, which is traditionally completed off campus, but they too are impacted as they wonder if the testing sites will be postponing Step 1 exams as they have Step 2 CS exams.
Our MS4s completed their rotations and interviews before travel restrictions and rotation cancellations began, but the culmination of medical school will look very different for their class than those who came before them. There wasn’t the traditional match day celebration. Many students feel uncertain of whether they will have a graduation ceremony.
Medical students have a unique position in this pandemic. While we want to be a resource in a potentially overwhelmed healthcare system and learn for future pandemics when we will be providers, we also recognize that we could become a burden to the system.
Students and providers alike--thank you to all those working to care for our community during this uncertain time.
By Monday night all inpatient rotations were canceled for medical students. By Tuesday all clinical rotations for 3rd and 4th year students--inpatient and outpatient---were canceled until at least March 31st in a nationwide decision by the AAMC and LCME.